How do I know if my child has Foetal Alcohol Spectrum Disorder?
Whilst there are a number of ways to identify if your child has FASD, it can be quite complicated to reach a conclusive decision. For many years medical professionals believed that 'facial dysmorphia' was essential to diagnose FASD, however today it is estimated that this appears in only 10% of cases. Below are some of the indicators to look for, however your child might have a few, or many of them:
- Low body weight
- Poor coordination
- Hyperactive behavior
- Difficulty with attention
- Poor memory
- Difficulty in school (especially with maths)
- Learning disabilities
- Speech and language delays
- Intellectual disability or low IQ
- Poor reasoning and judgment skills
- Sleep and sucking problems as a baby
- Chronic Otitis Media (Middle Ear Ache)
- Vision or hearing problems
- Problems with the heart, kidneys, or bones
- Shorter-than-average height
- Small head size
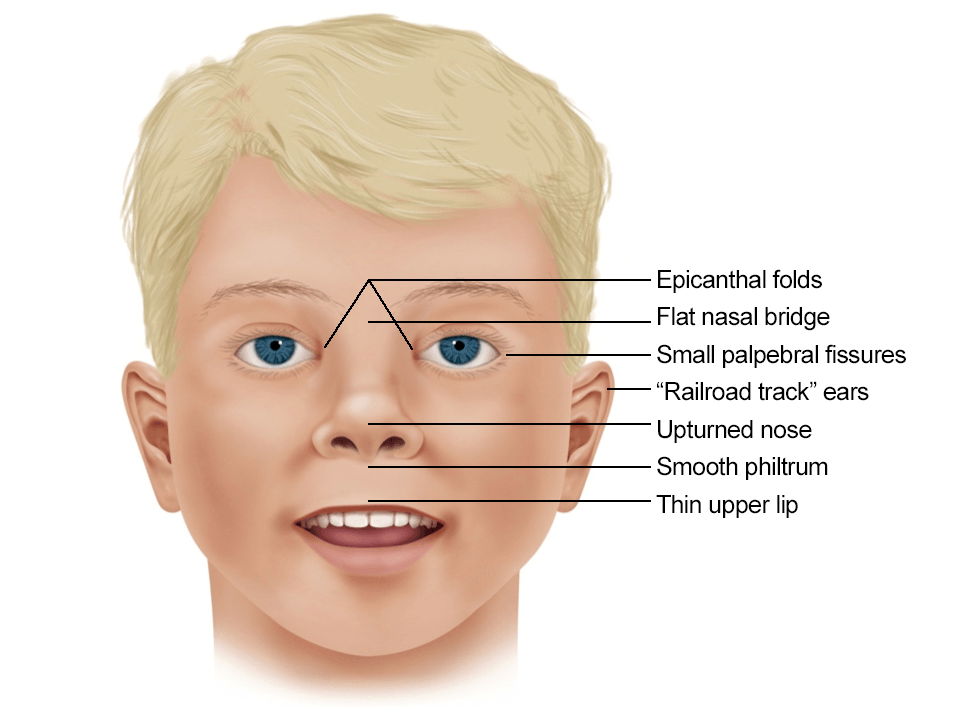
- Sentinel facial features (Image below)
The image above shows a range of facial dysmorphia that could suggest FASD
Approximately 10% of children with FASD will have sentinel facial features.
Most children will be diagnosed on the basis of their symptoms and evidence of prenatal alcohol exposure.